Nurse finds opportunity in WSU-Rochester's expanded master's programs
With projected 30 percent growth over the next decade, nurse practitioner is becoming one of the fastest growing professions in health care. The spike in demand is the result of an aging population, an anticipated doctor shortage, and new models of care that give nurse practitioners and physician assistants greater responsibility, especially in preventative care.
Here, in the shadows of one of the country’s greatest medical campuses, Winona State University-Rochester is working to train the next generation of nurse practitioners. The school now offers five master’s and graduate certificate programs in nursing, including nursing leadership and family nurse practitioner. A sixth area of focus, the Psychiatric-mental Health Program, is set to launch this summer.
The mental health program was set up following news that a local psychiatric inpatient unit was closing due to a lack of providers. “Acknowledging this need for providers, WSU Dean of Nursing Bill McBreen worked with graduate faculty to determine how WSU-R could create a viable solution for the Rochester community,” says university spokesperson Sam Beyers.
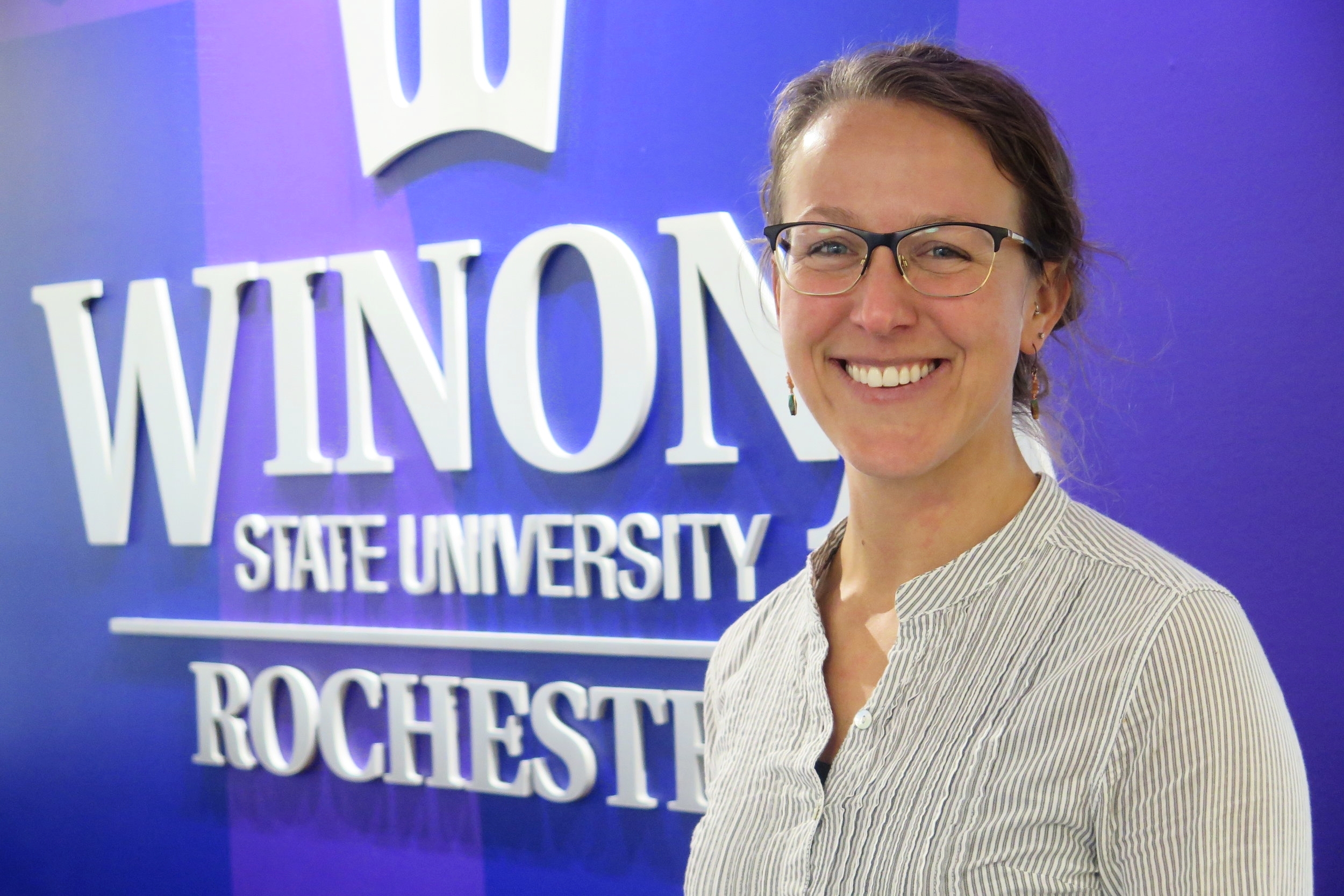
Brittany Mitchell will be part of the first pool of students to take the program. Already employed as an N.P. at Mayo Clinic, this is Brittany’s second time enrolling in courses at WSU-Rochester. Just last year, she graduated with her master’s degree in the Adult-Gerontology Acute Care Nurse Practitioner program.
Says Brittany, “My husband and I have conversations like, ‘what do you think you would do if you weren’t a nurse?’ And he has an answer within like 10 seconds. And I have no clue. I am a nurse.”
We recently sat down with the Mankato native to discuss her experiences as a student and nurse — and why she’s choosing to continue her education in the field of mental health.
Minor edits were made for flow and clarity.
This is now your second master’s program at WSU-R. What stood out from your first experience?
It was for sure the availability of clinical spots, [WSU-R] sets that up for you. And they help facilitate you getting those clinical hours, which is really hard in a lot of schools ... Another big sell for me was the face to face. I really love getting to know my professors and faculty. And everyone in my program that I graduated with, I still talk to; which is really nice because you’re going through a big life transition. And to have that small group of people who are going through the same thing is awesome.
What were your clinicals like?
What stood out about having that connection [with Mayo Clinic] is that the medical facility that you are doing clinicals at is a teaching facility. That’s their focus. That’s what they do. They do it all the time and they do it really well … So as a student, you go in thinking, ‘I’ll probably just observe.’ But every experience I had, I was considered part of the care team.
Why mental health this time?
First of all, the need for mental health is outrageous. Opportunities for what I can do in the future professionally will be huge. And also being dual certified; even I stay with my current role, mental health is in all of us. I mean, we all have struggles at some point. And I think with any patient I see, it would benefit my care and my practice to be able to incorporate mental health aspects.
Any advice for nurses who may be considering graduate school?
I would say do it — 100 percent, do it. Sometimes I get, ‘Oh you’re a nurse practitioner now.’ And no, I’m still a nurse and I will always be a nurse. That never, ever changes. It’s just a different way of providing care. Like now, instead of one-on-one supportive care, I am providing decision-making care. I am looking at an overall care plan and what type of medications or discharge necessities they patients haven’t coordinated on. So it’s just a different kind of nursing, and I think the way healthcare is going, the role of nurse practitioners is just going to grow.
Is there any one experience that made an impact on your career as a nurse?
I was doing a clinical at Mayo Clinic with the bone marrow transplant team. And there was a patient who was from out of state. She had gotten a bone marrow transplant, was there recovering, and obviously [experiencing] terrible, terrible pain. She wasn’t feeling well. She just wanted to leave. She wanted to go home.
And as a student, you have that extra little bit of time, because they have you focused on one or two patients, so you really get to know people. So I worked a few days in a row, and got to know her really, really well. I even knew about her family and stuff. And the transplant team I was working with was actually having me contribute, [such as] coordinating care for her going home. I was actually doing what I would be doing when I was done with school.
Then she had a complication and actually got real sick. I was able to go with her to a procedure she had to have done … And I think me being there and knowing her as a person gave her support and comfort going into a terrifying experience.
This article is part of a collection of interviews being published in partnership with Winona State University-Rochester.
Cover photo by Med City Beat